Decoding Atypical Pulmonary Arterial Hypertension: Unraveling Causes, Symptoms, and Modern Management Strategies
Decoding Atypical Pulmonary Arterial Hypertension: Unraveling Causes, Symptoms, and Modern Management Strategies
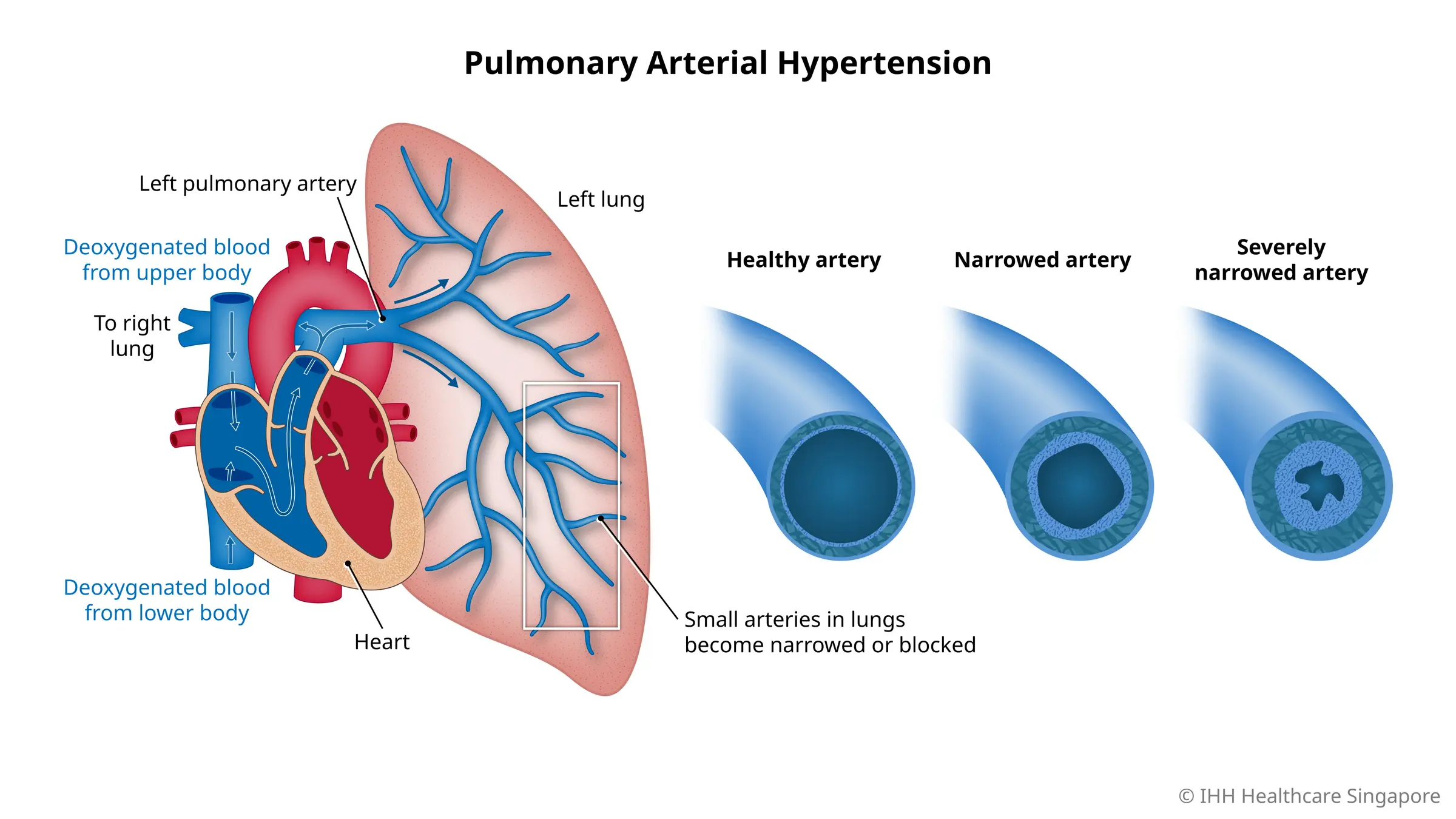
Atypical Pulmonary Arterial Hypertension (Atpl Disease), though clinically rare, represents a serious and progressive condition marked by elevated pressure in the arteries of the lungs, leading to right heart strain and, if untreated, life-threatening complications. Unlike standard pulmonary hypertension, Atpl often presents with ambiguous clinical features and insidious symptom onset, making early diagnosis a persistent challenge. Understanding its underlying causes, recognizing its subtle yet significant symptoms, and implementing evidence-based management approaches are critical to improving patient outcomes.
This article explores the pathophysiology, clinical presentation, and evolving treatment paradigms of Atpl Disease with a focus on actionable insights for healthcare providers and patients alike.
Unmasking the Causes: Complex Pathogenesis Behind Atypical Pulmonary Hypertension
The origins of Atpl Disease stem from a multifactorial interplay of genetic, environmental, and acquired factors that disrupt the delicate balance of pulmonary vascular homeostasis. While precise etiological triggers remain elusive in many cases, several key contributors have been identified through extensive clinical research.Genetic predisposition plays a foundational role, particularly in idiopathic forms. Mutations in genes regulating endothelial function and smooth muscle cell proliferation—such as *BMPR2* (bone morphogenetic receptor type 2)—are strongly associated with familial pulmonary arterial hypertension (PAH), a closely related clinical entity. “Patients with *BMPR2* mutations often show connective tissue abnormalities in pulmonary arteries, predisposing them to progressive vascular remodeling,” notes Dr.
Elena Vasquez, a pulmonary medicine specialist at the National Heart Institute. Environmental exposures also contribute significantly. Chronic illnesses—such as systemic connective tissue disorders (e.g., scleroderma, lupus), chronic lung diseases (e.g., chronic obstructive pulmonary disease, interstitial pneumonias), and congenital heart defects—frequently serve as underlying triggers.
Viral infections, especially those involving endotheliotropic agents, may initiate or exacerbate vascular injury. Immune dysregulation further amplifies risk, with autoimmune conditions promoting sustained vascular inflammation that accelerates disease progression. Autoimmune mechanisms are central to many Atpl cases.
In conditions like scleroderma-associated PAH, autoantibodies target pulmonary endothelium, prompting inflammatory cytokine release and endothelial dysfunction. This cascade promotes smooth muscle proliferation, intimal thickening, and medial hypertrophy—hallmarks of pulmonary artery stiffening and elevated resistance. Emerging evidence also highlights metabolic and epigenetic influences.
Mitochondrial dysfunction and aberrant methylation patterns may impair endothelial repair mechanisms, exacerbating vascular injury over time. These biological nuances underscore why Atpl Disease is not a singular condition but a spectrum influenced by diverse biological and lifestyle factors.
Identifying these varied causes demands a meticulous clinical evaluation.
Genetic screening and thorough assessment of comorbid conditions are increasingly essential in unraveling individual risk profiles and enabling early intervention.
Recognizing the Symptoms: Subtle Clues of Atypical Pulmonary Hypertension
The symptoms of Atpl Disease unfold gradually, often mimicking more common respiratory or cardiovascular conditions, which delays accurate diagnosis. This insidious progression underscores the need for heightened clinical awareness and a systematic approach to symptom evaluation. Early signs are frequently nonspecific but may include exertional dyspnea—shortness of breath that intensifies with activity—persistent fatigue, and unexplained weight loss.“Often, patients describe feeling winded climbing a few flights of stairs or walking up a slight incline,” observes Dr. James Lin, a leading pulmonologist. “These are red flags long before overt hemodynamic failure.” Beyond exertional symptoms, systemic indicators demand attention.
Chronic cough, chest pressure or pain, and palpitations may emerge as pulmonary vascular resistance increases. Some patients report syncope during strenuous exertion, a potential sign of right heart compromise. Over time, the severity of these manifestations correlates with disease progression and right ventricular dysfunction.
As hypertension advances, physical findings become more pronounced: peripheral edema—swelling in the lower extremities due to right-sided heart failure; a Hitchenson’s sign—lateral chest wall protrusion in right lateral decubitus views; and a prominent third heart sound (triple systolic murmur) indicating elevated pulmonary pressures. Brain fog and reduced exercise tolerance further compound daily life, often mistaken for anxiety or deconditioning. More insidious is the risk of sudden cardiac decompensation, particularly during physical stress or infection, underscoring the importance of regular monitoring in at-risk individuals.
“Early recognition hinges on integrating symptom patterns with objective data—echocardiography, pulse wave analysis, and 6-minute walk tests are indispensable,” says Dr. Vasquez. “Months of unrecognized symptoms precede clinical deterioration, so patient education about evolving signs is vital.”
Timely symptom awareness empowers both patients and clinicians to act before irreversible vascular changes occur.
Integrating Diagnosis, Treatment, and Long-Term Management of Atpl Disease
Diagnosing Atpl Disease requires a multidisciplinary approach, leveraging advanced imaging, functional testing, and biomarker profiling.While no single test confirms the diagnosis, a constellation of findings guides clinical certainty. Echocardiography serves as the initial screening tool, identifying elevated pulmonary artery systolic pressure (usually >25 mmHg at rest) and right ventricular hypertrophy. Pulmonary function tests assess underlying lung pathology, while high-resolution CT scans reveal vascular remodeling and parenchymal abnormalities.
Definitive diagnosis often relies on right heart catheterization, which remains the gold standard. This invasive procedure measures pulmonary artery pressure, cardiac output, and vascular resistance while enabling simultaneous assessment of hemodynamic compromise. ” “Without invasive confirmation, atypical presentations risk misdiagnosis,” warns Dr.
Lin. “A careful exclusion of chronic lung disease, left heart failure, and other secondary causes is imperative before attributing symptoms to Atpl.” Management strategies evolve with disease severity and patient profile. The cornerstone of therapy lies in targeted pharmacological interventions designed to reduce pulmonary vascular resistance, improve cardiac output,
:max_bytes(150000):strip_icc()/EVERGREEN-7MostCommonCausesofPulmonaryArterialHypertension-final-5a884b6f2a0c4f24bf8871af2378aa8d.png)


Related Post

Gun Flipper Unblocked: Breaking Barriers in a Digital Showdown

The Enduring Legacy of Paula Hurd: A Life Defined by Media, Insight, and Timeless Influence
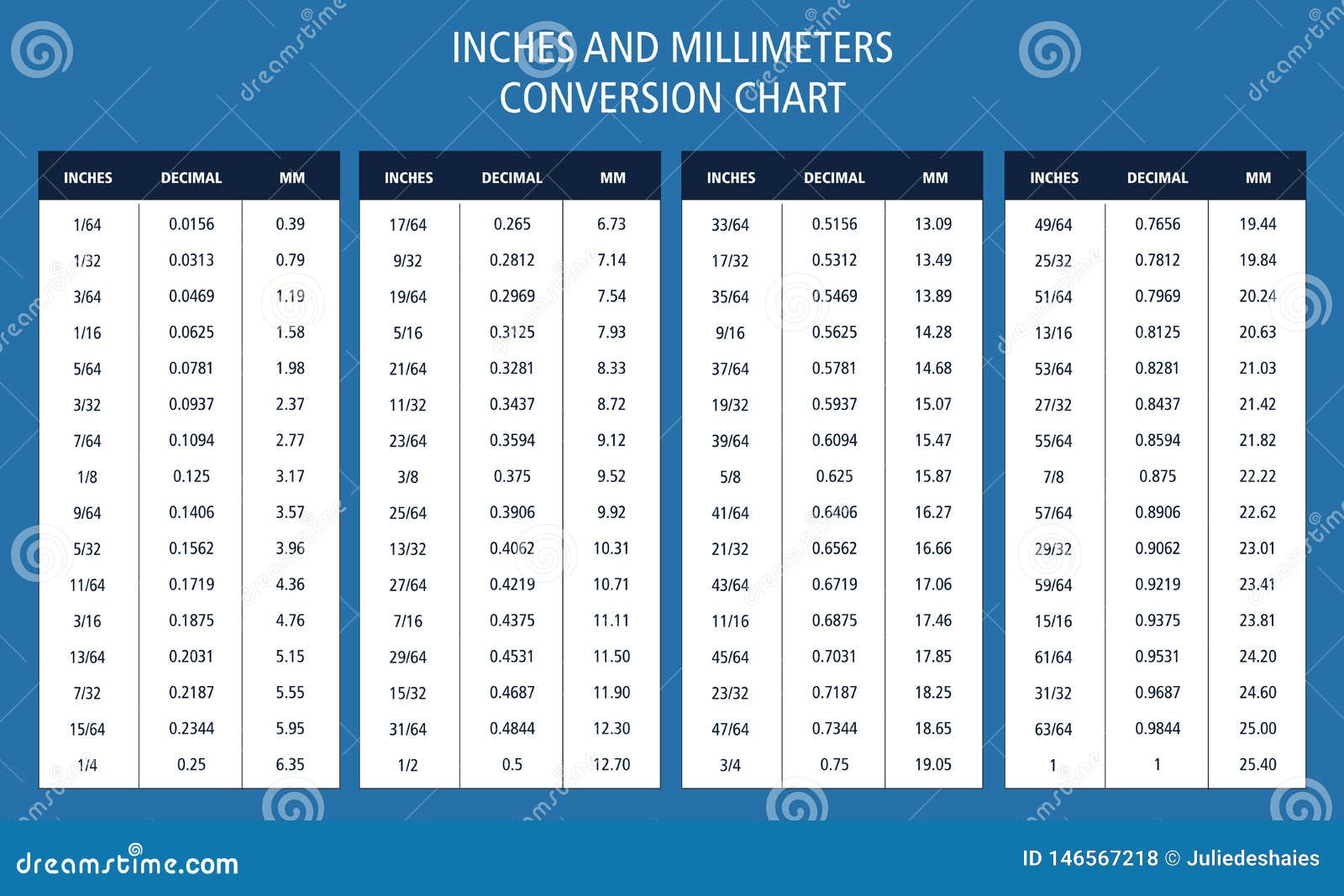
45 Millimeters to Inches: The Precision Conversion That Shapes Global Standards
/south-carolina-state-county-map-165047526-58b9dacd3df78c353c4410c6.jpg)
IOSCDONNASC Police: What You Need to Know Before Rolling Into South Carolina’s Counties

