From Ancient Warnings to ICD-10: The Evolution of Hypertension Diagnosis
From Ancient Warnings to ICD-10: The Evolution of Hypertension Diagnosis
Long before modern medicine categorizes high blood pressure, civilizations recognized the silent threat of elevated arterial force—linking symptoms to systemic damage long before the science caught up. Today, the ICD-10 classification system stands as the global standard for diagnosing and documenting hypertension, enabling precise tracking of one of the world’s most pervasive cardiovascular risks. This evolution from crude observation to structured coding reflects how medical understanding and diagnostic precision have transformed over centuries, ultimately shaping prevention, treatment, and public health policy worldwide.
The Origins of Hypertension Recognition: From Humoral Theories to 19th-Century Challenges
Ancient physicians, including Greek and Chinese healers, identified bodily imbalances resembling hypertension long before the term existed.
In the 1600s, English physician Thomas Sydenham noted “excessive tension” in patients displaying headaches and fatigue—early ironic descriptions of symptoms now linked to elevated blood pressure. However, effective measurement was decades away. Before the 1800s, diagnosable tools were nonexistent; physicians relied on pulse palpation, subjective reports, and oftentimes fatal assumptions about chronic symptoms.
As cardiovascular researcher Sir Richard Bright observed in the early 1800s, “The blood’s weight is not always visible, yet its burden leaves lasting marks.”
The Birth of Measurement: Sphygmomanometry and the First Steps toward Precision
The turning point came in the late 1800s with the invention of the sphygmomanometer. In 1881, French physician Jean-Louis-Philippe Poiseuille refined mercury pressure devices, establishing systolic and diastolic values—foundational for later classification. Yet standardization remained elusive.
By the early 1900s, circadian patterns and target organ damage were emerging as diagnostic clues, but absence of uniform terminology hindered global reporting. As hypertension specialist Dr. Paul C.
Clement noted, “Without a shared language, even the most critical signs remained isolated fragments.”
ICD-10 Adoption: Standardizing Hypertension Across Borders
The International Classification of Diseases, 10th Revision (ICD-10), developed by the World Health Organization (WHO) and first implemented in 1992, provided the critical framework for unifying hypertension diagnosis. Unlike earlier systems, ICD-10 introduced specific codes under the broader “I70 series” categories, enabling clinicians and researchers worldwide to classify hypertension with unprecedented accuracy. Key diagnostic criteria include:
- Blood pressure ≥140/90 mmHg on at least two occasions, confirmed through repeated measurements.
- Subcategories: Essential (primary) hypertension (accounting for ~90% of cases) and secondary forms (due torenal disease, endocrine disorders, or medications).
- Documentation of target organ damage (e.g., left ventricular hypertrophy, retinopathy) when present to stratify risk.
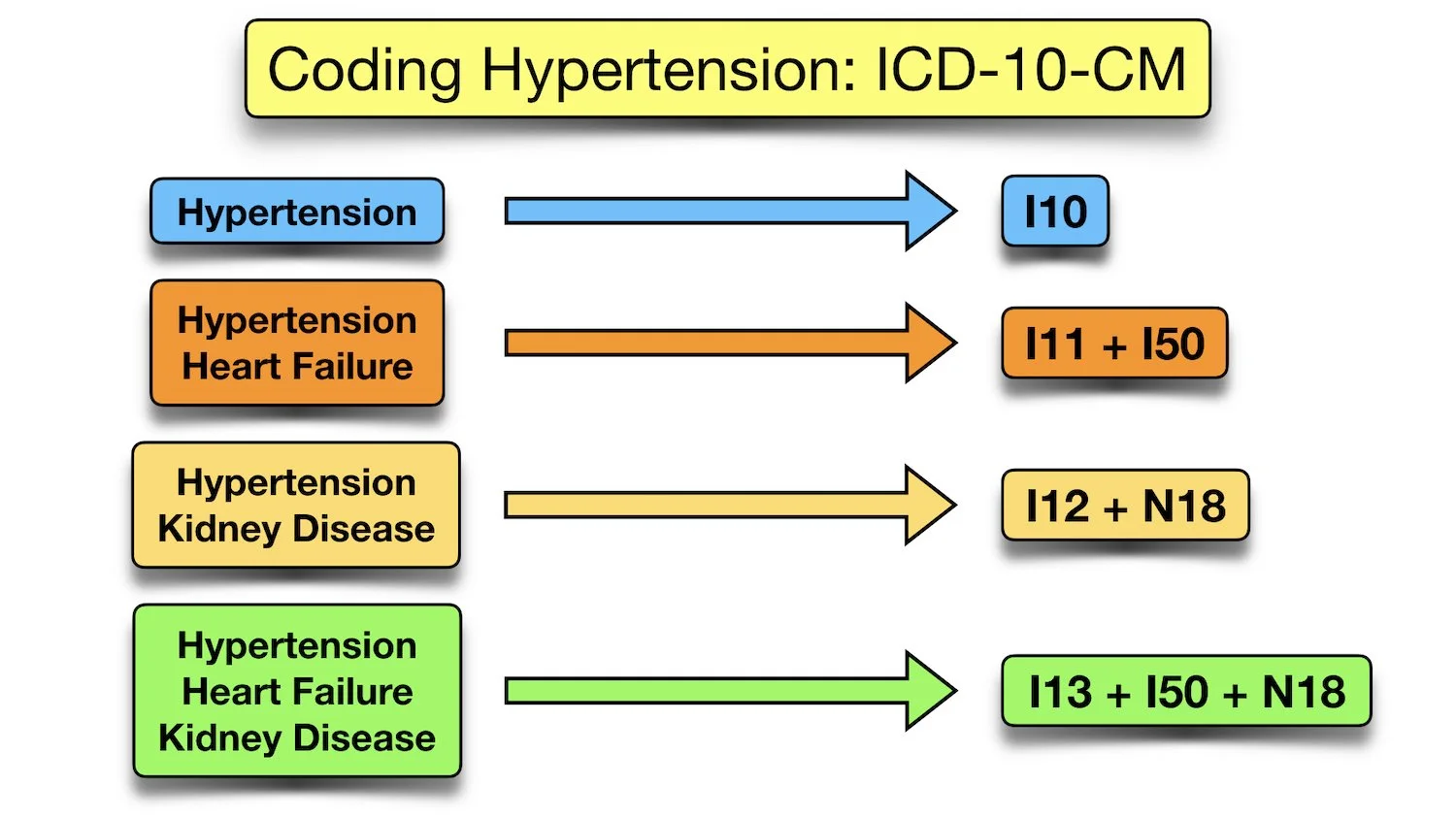
ICD-10 codes—such as I10 for essential hypertension—bridge clinical practice and epidemiology, allowing precise tracking of prevalence, complications, and treatment outcomes across populations.
This level of granularity supports everything from patient care to national health surveillance.**
Impact of ICD-10 on Clinical Practice and Public Health
The integration of ICD-10 into electronic health records revolutionized hypertension management. Gone are ambiguous notes and inconsistent reporting—clinicians now log diagnoses with specificity, enabling real-time alerts for threshold readings and timely interventions. In primary care, this translates to earlier identification of high-risk patients, while cardiologists leverage ICD-10 data for risk stratification models.
Public health initiatives benefit equally: standardized coding lets governments monitor hypertension trends, allocate resources, and evaluate population-level interventions like sodium reduction campaigns or screening programs.
According to the WHO, “ICD-10 transformed hypertension from an underreported risk into a measurable, actionable public health challenge.” This shift underpins modern guidelines—such as those from the American College of Cardiology and the European Society of Cardiology—where early diagnosis via precise coding leads to more effective prevention strategies.
From Names to Numbers: The Code Behind the Crisis
ICD-10’s structured classification enables deeper analysis of hypertension’s global burden. For example, I16.9 (hypertensive emergencies) isolates acute crises requiring urgent care, while I11 (chronic hypertension with heart failure) guides long-term monitoring protocols. These codes do more than classify—they reveal patterns.
Analysis of ICD-10 data across Europe, for instance, uncovered rising prevalence in younger adults, prompting revised screening age thresholds in several countries.
Moreover, the clarity of ICD-10 supports billing, insurance approval, and research funding. In a world where data drives policy, the system ensures that every hypertension case contributes to a coherent, actionable global narrative.
The Scientific and Human Evolution Behind Hypertension Classification
The story of hypertension classification through ICD-10 illustrates how medical progress thrives on both technological innovation and conceptual rigor. While ancient texts whispered of blood’s weight, today’s WHO code transforms vague symptoms into quantifiable risk factors.
As hypertension expert Dr. Katharineウェア emphasizes, “Classification is not just about labels—it’s about unlocking insights that save lives.” Each ICD-10 code is a milestone in understanding the nuanced nature of high blood pressure, empowering clinicians, researchers, and policy makers alike to act decisively.
From speculative symptoms to structured healthcare metrics, the journey of hypertension diagnostics reflects humanity’s enduring quest to decode invisible threats. With ICD-10 as the crystallizing achievement, this legacy continues to shape how we detect, manage, and ultimately confront one of medicine’s longest-standing battles—a battle won not in silence, but through precise classification.

Related Post

Unlocking the Mystery: What’s an Arch Picture and Why It Matters

Sunuk Com: A Comprehensive Overview of a Emerging Industrial Powerhouse

How Many Oz in Half a Pound? The Clear Answer Every Kitchen Enthusiast Needs

Ethan Klein Cough: Unraveling the Science Behind a Painful Reflex That Shapes Human Health

