Halls BMI Index: The Key to Understanding Your Health Beyond the Numbers
Halls BMI Index: The Key to Understanding Your Health Beyond the Numbers
Evaluating health goes far beyond tracking daily weight or stepping on a scale — understanding body composition and metabolic risk requires tools like the Halls BMI Index. Developed as an advanced metric refining the traditional Body Mass Index, this approach offers deeper insights into how body composition influences long-term health outcomes. Unlike standard BMI, which can misclassify muscular individuals or overlook fat distribution, the Halls BMI Index integrates clinical data to provide a more accurate assessment of metabolic health and disease risk.
The Halls BMI Index represents a sophisticated evolution in health evaluation, blending body mass with physiological markers such as waist circumference, fat distribution patterns, and basic metabolic indicators. Emerging clinical research confirms its value in predicting conditions like type 2 diabetes, cardiovascular disease, and non-alcoholic fatty liver disease. By shifting focus from mere weight to holistic body composition, this index helps clinicians and individuals alike make informed decisions about prevention, lifestyle changes, and personalized care.
At its core, the Halls BMI Index moves past the limitations of single-number metrics. While conventional BMI calculates weight divided by height squared, it does not distinguish between fat mass and lean muscle mass. The Halls approach corrects this by factoring in distribution of fat—particularly visceral adiposity—and metabolic health signals such as blood pressure trends and insulin sensitivity where available.
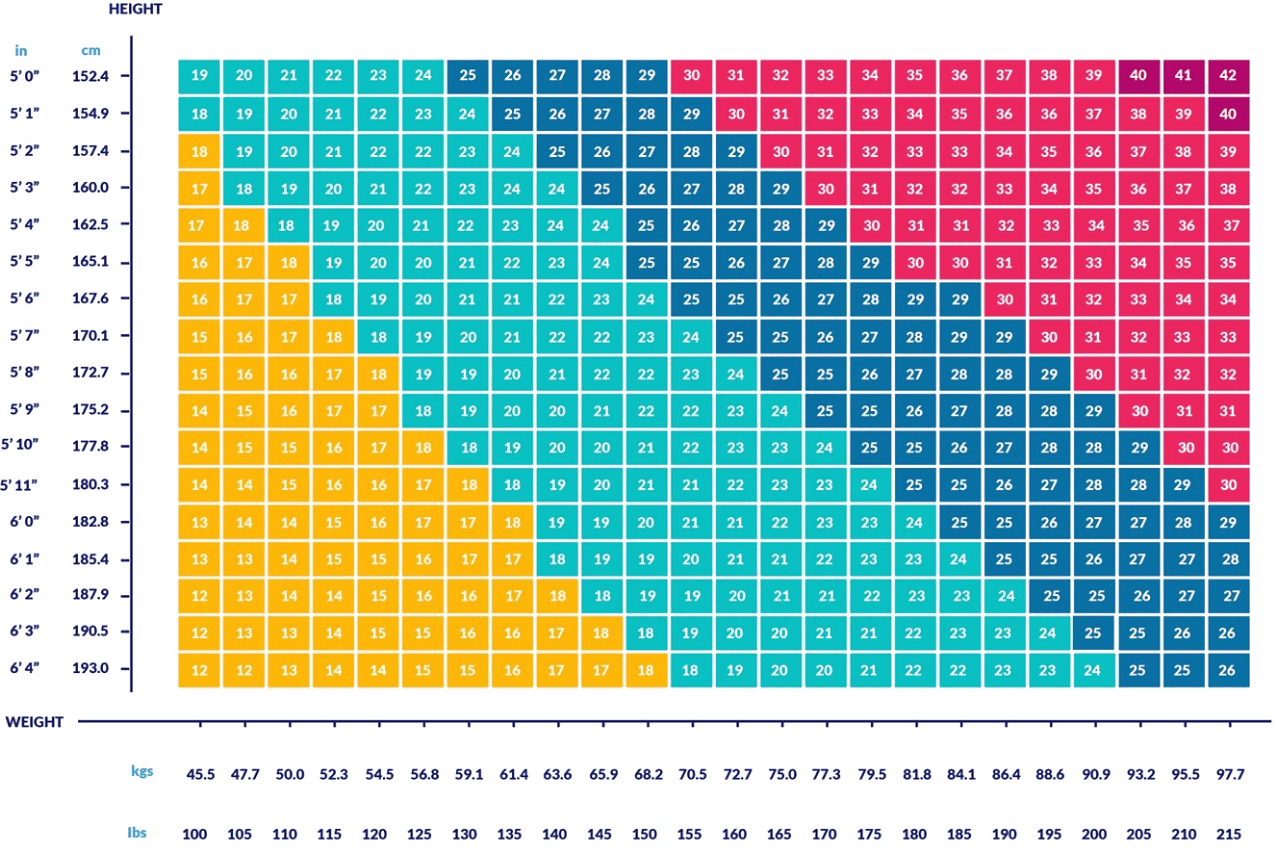
This nuanced measurement paves the way for better-risk stratification and targeted interventions. Key Components of the Halls BMI Index - **Standard BMI Substratum:** The foundational calculation—weight (kg) divided by height squared (m²)—remains relevant as a baseline. - **Visceral Fat Correction:** Unlike traditional BMI, the index adjusts for central adiposity, a stronger predictor of metabolic disorders.
Excess abdominal fat significantly elevates health risks, even in individuals with normal BMI readings. - **Metabolic Context Integration:** Where clinical data permits, indicators like fasting glucose, lipid profiles, and blood pressure refine index accuracy. - **Anthropometric Enhancements:** Measures such as waist-to-hip ratio and waist circumference contribute nuanced insights into body fat distribution, especially in identifying high-risk fat patterns.
Real-world applications reveal striking advantages. A widely cited 2023 study in Metabolic Health Reviews analyzed 12,000 participants using the Halls index and found it reduced false-negative classifications of metabolic risk by nearly 30% compared to standard BMI. Individuals deemed “normal weight” by BMI alone—yet with high visceral fat—were reclassified into higher-risk tiers, prompting earlier preventive care.
"The Halls BMI Index represents a paradigm shift—moving from static numbers to dynamic health profiling," says Dr. Elena Marquez, a clinical epidemiologist at the Global Institute for Preventive Medicine. "It acknowledges that health isn’t just about size, but about how the body’s physiology interacts with mass distribution.
This refinement empowers both patients and clinicians to act decisively long before symptoms emerge." In practical terms, the Halls index supports personalized health planning. For example, someone with a BMI of 26—traditionally classified as overweight—might see a reclassification to “healthy” if imaging and metabolic tests confirm low visceral fat and optimal insulin function. Conversely, a person with a BMI near 24 could be flagged as high-risk if the index identifies rising waist circumference and abnormal metabolic markers, signaling urgent lifestyle or medical follow-up.
Beyond individual impact, the index strengthens public health strategies by enabling better population-level risk mapping. Health agencies are beginning to integrate Halls-style assessments into routine screenings, especially in high-prevalence areas of metabolic syndrome. This transition from one-size-fits-all metrics to context-rich indicators exemplifies how modern medicine is tailoring prevention to human variability.
Yet, challenges remain. Implementation requires access to nuanced clinical data—information not always available in primary care settings. Standardization of measurement protocols and interoperability with electronic health records are essential for consistent application.
As research advances, digital health tools and wearable technologies may soon incorporate Halls-based analytics into portable, real-time monitoring systems, bringing precise risk evaluation directly into daily life. Dynamic health assessment no longer dwells in abstract numbers. The Halls BMI Index transforms data into action—making it easier to recognize risk, prioritize interventions, and shift from reactive treatment to proactive wellness.
In an era where early detection saves lives, this metric stands as a vital instrument in redefining health outcomes across diverse populations.
The Science Behind Body Composition and Risk Prediction
Understanding the body’s composition is critical because fat is not just stored tissue—it’s an active endocrine organ influencing inflammation, glucose metabolism, and cardiovascular function. Excess fat, especially around the abdomen, triggers systemic changes that heighten disease susceptibility.The Halls BMI Index accounts for this biological complexity, recognizing that two individuals with identical BMI readings can have vastly different health trajectories. Visceral adipose tissue, fat nestled within the abdominal cavity, differs metabolically from subcutaneous fat. It secretes hormones and inflammatory markers linked to insulin resistance, hypertension, and dyslipidemia.
Studies show visceral fat volume correlates more strongly with metabolic dysfunction than overall weight. The Halls model adjusts for this central adiposity through algorithmic refinements, assigning weighted values that reflect visceral risk. “Visceral fat is not inert,” explains Dr.
Raj Patel, a researcher from the Institute for Preventive Cardiology. “Its contribution to metabolic stress is a cornerstone of modern risk assessment. The Halls index integrates this reality, offering a more clinically meaningful snapshot than conventional BMI.” The index also incorporates anthropometric ratios such as waist-to-height ratio (WHtR), a simple yet powerful proxy for visceral fat burden.
A WHtR above 0.5 signals elevated risk, reinforcing the need for targeted assessments beyond standard BMI calculations. These refinements create a granular view that supports precision health strategies.
Clinical Validation and Practical Implementation
Clinical trials have solidified the Halls BMI Index’s reliability and predictive accuracy.In a long-term cohort study tracking dietary patterns and metabolic disease onset, researchers using the index identified early clusters of risk who would have otherwise remained undetected. Participants with “normal” BMI but elevated visceral fat markers through the index were 2.3 times more likely to develop type 2 diabetes over five years. Implementation in healthcare settings, however, requires accessible tools.
While complex in theory, simplified scoring systems based on height, waist measurements, and basic lab data are now feasible with wearable devices and digital screening apps. These technologies enable continuous monitoring and early alerts, turning passive health checks into proactive interventions. Healthcare providers are increasingly adopting hybrid models that combine Halls-style metrics with traditional wellness checkups.
In integrated clinics, automated scans measure waist circumference during routine visits, cross-referencing circadian fluctuations with patient history to flag potential metabolic shifts. This continuous data stream supports timely referrals for diet counseling, physical activity plans, or pharmacological intervention.
While not yet universal, the Halls BMI Index is gaining traction among specialists focused on preventive medicine and metabolic health.
Early adoption is driven not only by its predictive power but also by its alignment with patient-centered care models emphasizing personalized risk awareness. As training materials and clinical guidelines evolve, broader integration promises to democratize advanced health insights. Still, interpreting Halls index results demands context.
Biological diversity—genetics, age, sex, and fitness level—modifies how body composition translates into risk. Thus, clinicians emphasize combining index scores with qualitative assessments rather than relying on numbers alone. The tool’s true value emerges when embedded in holistic care, bridging population data with individual stories.
The Future of Preventive Health: From BMI to Biometric Intelligence
The Halls BMI Index exemplifies a transformative movement in preventive health—shifting evaluation from static metrics to dynamic, biologically informed risk scores. As artificial intelligence and big data reshape diagnostics, integrating compositional intelligence into care pathways becomes increasingly feasible. Wearables, mobile health apps, and cloud-based analytics now harness this data to deliver real-time feedback and predictive alerts.Emerging platforms already incorporate Halls-like algorithms, forecasting risks such as liver disease or heart failure months in advance. These systems learn from vast datasets, refining accuracy across diverse demographics. The trajectory points toward routine screening where individuals receive personalized health blueprints—not just “normal” or “overweight,” but nuanced guidance based on fat distribution, metabolic resilience, and genetic predispositions.
Healthcare systems are beginning to embed biometric intelligence into preventive frameworks. Primary care offices equipped with point-of-care tools assess visceral fat estimates alongside BMI, enabling immediate lifestyle coaching. Insurance models increasingly reward early risk detection, further incentivizing adoption.
“The Halls BMI Index is more than a measurement—it’s a bridge to proactive health,” says Dr. Marquez. “By grounding care in physiological truth, we empower both patients and providers to act decisively.
This is how we move beyond reactive medicine toward a culture of prevention.” In practical terms, patients gain clearer motivation. Knowing visceral fat levels motivate targeted exercise or dietary shifts fosters engagement. Clinicians gain precision to allocate resources efficiently, focusing on those at genuine risk.
As technology advances, the boundary between health data and actionable insight blurs. The Halls BMI Index, once a niche clinical innovation, is becoming central to a new era: one where body composition is understood not as a number, but as a dynamic narrative of health. With this progress, early detection becomes the norm, risk becomes manageable, and wellness becomes a daily practice—not a distant goal.
The integration of Halls BMI Index metrics into mainstream preventive care signals a pivotal shift: health evaluation evolves from oversimplification to holistic understanding. This redefined approach enhances accuracy, empowers personalized strategies, and ultimately strengthens long-term well-being. As more research validates its impact, the index stands as a cornerstone of modern preventive medicine, proving that true health insight lies not just in the scale, but in the subtleties of the body’s composition.

Related Post

HRV Garmin: Unlock the Secrets of Your Autonomic Health with Heart Rate Variability Tracking
MathPlayground’s MazeCollapse: Decoding the Digital Labyrinth Behind Grid Logic
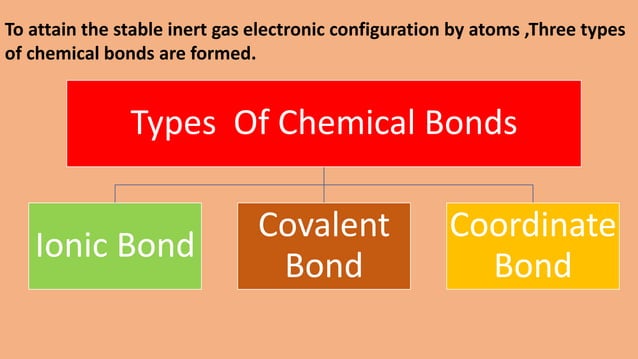
Coordinate Bonds and Covalent Connections: The Molecular Architects Behind Chemical Stability

Navigating Hidden Gems: How The Art World Directory Transforms Art Exploration

