Mucinous Ovarian Cancer: Rising Silently, Demanding Awareness
Mucinous Ovarian Cancer: Rising Silently, Demanding Awareness
Mucinous ovarian cancer—though less common than its epithelial counterparts—accounts for nearly 20% of all ovarian malignancies and remains one of the most underdiagnosed and aggressive forms of the disease. Rarely detected in early stages due to subtle symptoms and anatomic complexity, this cancer type often evades routine screening, leaving patients with poorer prognoses when diagnosis finally occurs. Understanding mucinous ovarian cancer—its biology, risk factors, warning signs, and latest advances—is essential not only for early detection but for shaping better treatment strategies and improving survival outcomes.
The Silent Threat: What Makes Mucinous Ovarian Cancer Unique
Unlike most high-grade serous carcinomas, which tend to be swiftly progressive, mucinous ovarian cancers derive from epithelial cells in the ovary’s surface lining and produce excess mucus, contributing to both pathogenesis and diagnostic challenges. Histologically, these tumors are defined by clusters of mucin-producing cells embedded in a thick, often thickate stroma, a feature visible under the microscope but not always detectable via standard imaging or blood tests. "One of the biggest hurdles in managing mucinous ovarian cancer," notes Dr.Elena Marquez, a gynecologic oncologist at Memorial Sloan Kettering, "is its insidious onset—symptoms mimic common gastrointestinal or abdominal discomfort, leading to years of delayed diagnosis." - Bloating - Abdominal distension - Early satiety - Altered bowel habits - Pelvic pressure - Irregular bleeding These nonspecific signs frequently prompt misdiagnosis as irritable bowel syndrome or ovarian cysts, allowing the cancer to grow undetected. Once advanced, mucinous tumors demonstrate aggressive local invasion and a higher likelihood of early peritoneal spread, undermining surgical curability.
Who Is At Risk?
Recognizing Key Risk Factors While the precise causes of mucinous ovarian cancer remain under investigation, several risk factors have emerged through epidemiological studies. Age is a primary factor—most cases occur in women over 50, with a median age at diagnosis of 58 years. However, rare early-onset cases have been reported in younger women, underscoring genetic variability.
Family history looms large: women with Lynch syndrome—an inherited condition caused by mismatch repair gene mutations—face a substantially elevated risk, with mucinous tumors occurring up to 10 times more frequently than in the general population. Polycystic ovary syndrome (PCOS) and endometriosis also appear to increase susceptibility, possibly due to chronic ovarian stimulation and hormonal imbalances. Environmental influences, including prolonged oral contraceptive use and toxin exposure, remain less defined but warrant further study.
Unlike epithelial ovarian cancers, mucinous subtypes show limited association with traditional risk factors like smoking, indicating a need for targeted surveillance strategies within high-risk cohorts.
Diagnosing the Unseen: Challenges and Screening Strategies
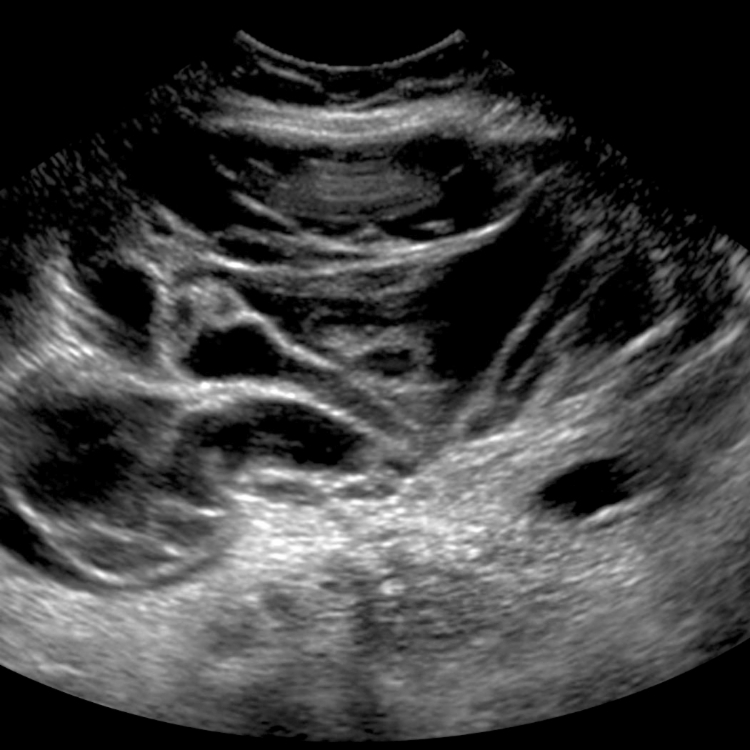
Diagnosing mucinous ovarian cancer begins with recognizing its diagnostic ambiguity. The tumor’s mucinous nature means it often lacks the dramatic serum biomarker spikes—like CA-125—that guide detection for other ovarian cancers.While CA-125 may rise, its sensitivity and specificity are suboptimal in mucinous cases, limiting its utility as a standalone screening tool. Imaging modalities such as transvaginal ultrasound help identify complex adnexal masses but cannot reliably distinguish mucinous from other subtypes. Histopathology remains the gold standard, requiring surgical biopsy and tissue analysis.
Specialized staining techniques, including mucicarmine and periodic acid-Schiff (PAS), reveal abundant intracytoplasmic mucin, confirming diagnosis. Emerging research focuses on blood-based biomarkers and molecular profiling to improve early detection. Circulating tumor DNA and glycoproteins unique to mucinous cells are under investigation, offering hope for non-invasive screening in the future.
Meanwhile, gynecologic clinicians are urged to maintain vigilance in patients with known risk factors, especially when symptoms persist beyond typical benign causes.
From Diagnosis to Treatment: Navigating Mucinous Ovarian Cancer Therapy
Once diagnosed, mucinous ovarian cancer presents distinct therapeutic challenges. Histologically, these tumors often display intermediate grade patterns, neither purely benign nor overtly aggressive—yet their tendency for early peritoneal dissemination demands aggressive intervention.Standard management typically combines surgery and chemotherapy, but response rates vary, guided by molecular subtyping. "Because mucinous tumors frequently carry distinct genetic alterations, such as KRAS or TP53 mutations, tailoring therapy is critical," emphasizes Dr. Marquez.
"We’re beginning to see better outcomes with regimens combining platinum-based chemotherapy, intraperitoneal agents, and emerging targeted therapies like mTOR inhibitors." Surgical options demand careful evaluation: wide-ranging cytoreductive surgery aims to remove all visible disease, but complete resection remains elusive in many cases. In advanced stages, prevention of recurrence hinges on ongoing systemic treatment and close monitoring. Research is actively probing immunotherapies and personalized medicine, particularly for recurrent disease.
Trials exploring PARP inhibitors in BRCA-mutated mucinous cancers show promise, though uptake in clinical practice lags due to tumor biology differences compared to serous variants.
What Patients and Practitioners Need to Know: Empowerment Through Knowledge
For women and clinicians alike, recognizing mucinous ovarian cancer begins with awareness. Unlike earlier-p subscribers, which often trigger rapid evaluation, mucinous disease tactfully disguises itself among common gastrointestinal or hormonal concerns.Trusting persistent, unexplained symptoms—even in the face of benign reassurance—can be life-saving. Education remains key. Women with Lynch syndrome or strong family histories should discuss genetic testing proactively during reproductive and preventive care visits.
Clinicians, in turn, must maintain a high index of suspicion in older patients with inhabitual abdominal symptoms unresponsive to usual treatments. Multidisciplinary care—uniting gynecologic oncologists, pathologists, radiologists, and genetic counselors—ensures timely, precise diagnosis and treatment planning. Patient advocacy groups and educational resources further amplify early detection, reducing mortality through shared knowledge.
In sum, mucinous ovarian cancer is a formidable yet increasingly tractable adversary. Its silent progression and diagnostic elusive nature demand heightened vigilance, but advances in pathology, molecular diagnostics, and targeted therapies are shifting outcomes. Awareness, timely action, and comprehensive care form the foundation of hope—turning silence into response, and risk into resilience.



Related Post

Women’s Cricket World Cup Schedule: When to Watch, Who’s Watching, and the Global Journey of the Game

Is India Married? Inside the Surprising Personal Journey and Career Triumphs That Redefine Glamour

Top Karaoke Songs for Guys That Demand the Stage

Unlock Math Mastery: How Ti Nspire Online Transforms Classroom Learning