Parietal vs Visceral Pleura: The Dynamic Dialogue Of Lung Protection And Pulmonary Defense
Parietal vs Visceral Pleura: The Dynamic Dialogue Of Lung Protection And Pulmonary Defense
Beneath the surface of human respiration lies a carefully orchestrated battle between two specialized membranes: the parietal pleura and the visceral pleura. Though often overlooked, these thin yet resilient layers are central to how the lungs function safely within the chest cavity. Their structural differences and coordinated biology underpin critical aspects of pulmonary health, disease prevention, and surgical outcomes.
Understanding their distinct roles not only illuminates the mechanics of breathing but also reveals how disruptions in their integrity can lead to serious clinical complications.
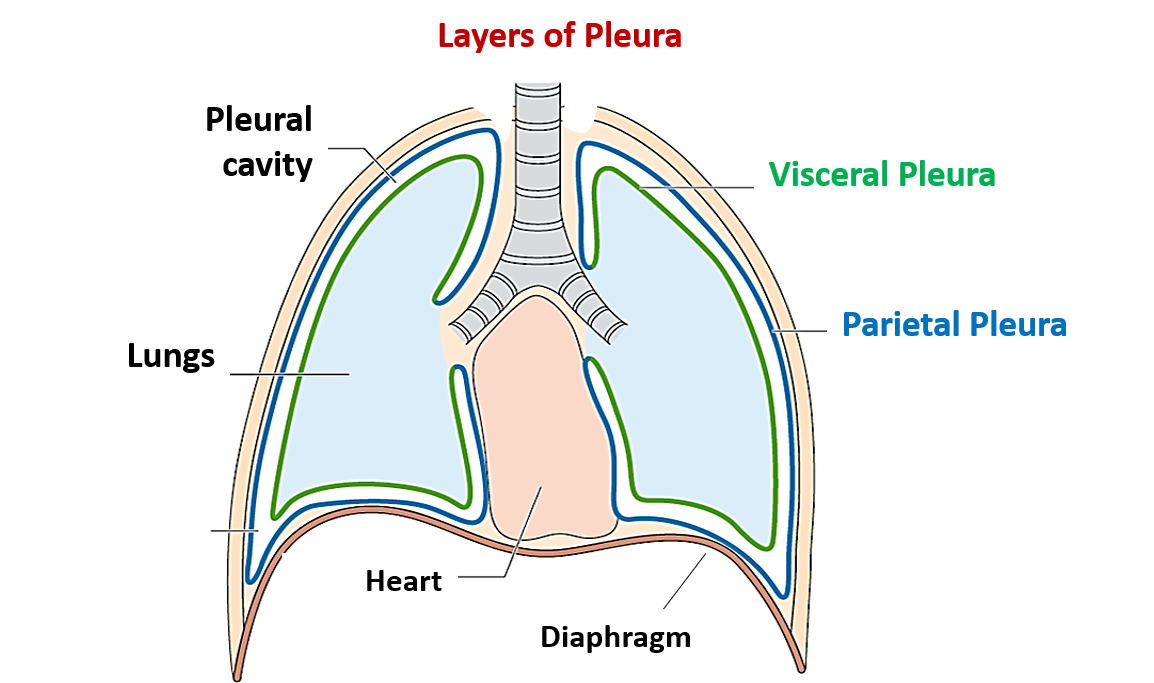
The parietal pleura lines the inner surface of the thoracic cavity walls, diaphragm, mediastinum, and visceral thoracic structures, while the visceral pleura completely covers the lung surfaces—both adherent yet distinct in function. This anatomical separation enables a controlled gliding motion essential for normal respiration, but their protective roles extend far beyond mere friction reduction.
The pleural layers collectively form a sealed barrier that maintains negative intrapleural pressure, a key physicist principle that keeps the lungs perpetually inflated during the breathing cycle.
Each pleural layer serves a unique physiological purpose. The parietal pleura detects pain through robust sensory nerve innervation, making it critical in diagnosing pleuritic conditions such as pneumonia, pleural effusion, or mesothelioma. Because sensory nerves are concentrated in its base and peripheral edges, irritation here often produces referred pain—common in pneumothorax or lung tumor encroachment.
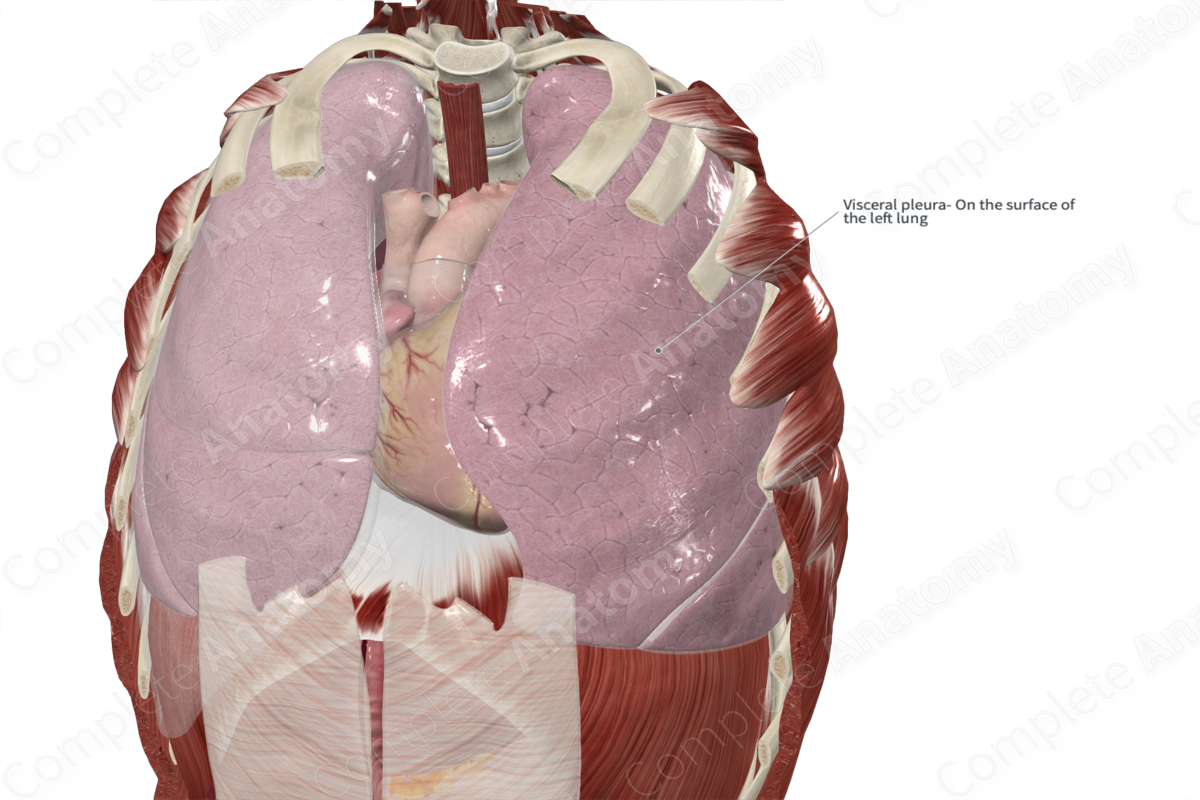
“Visceral pleura, innervated by autonomic fibers, is largely insensitive to pain,” notes Dr. Elena Petrova, pulmonologist at Johns Hopkins Hospital. “Its injury may only become apparent when parietal pleural tension is altered.”
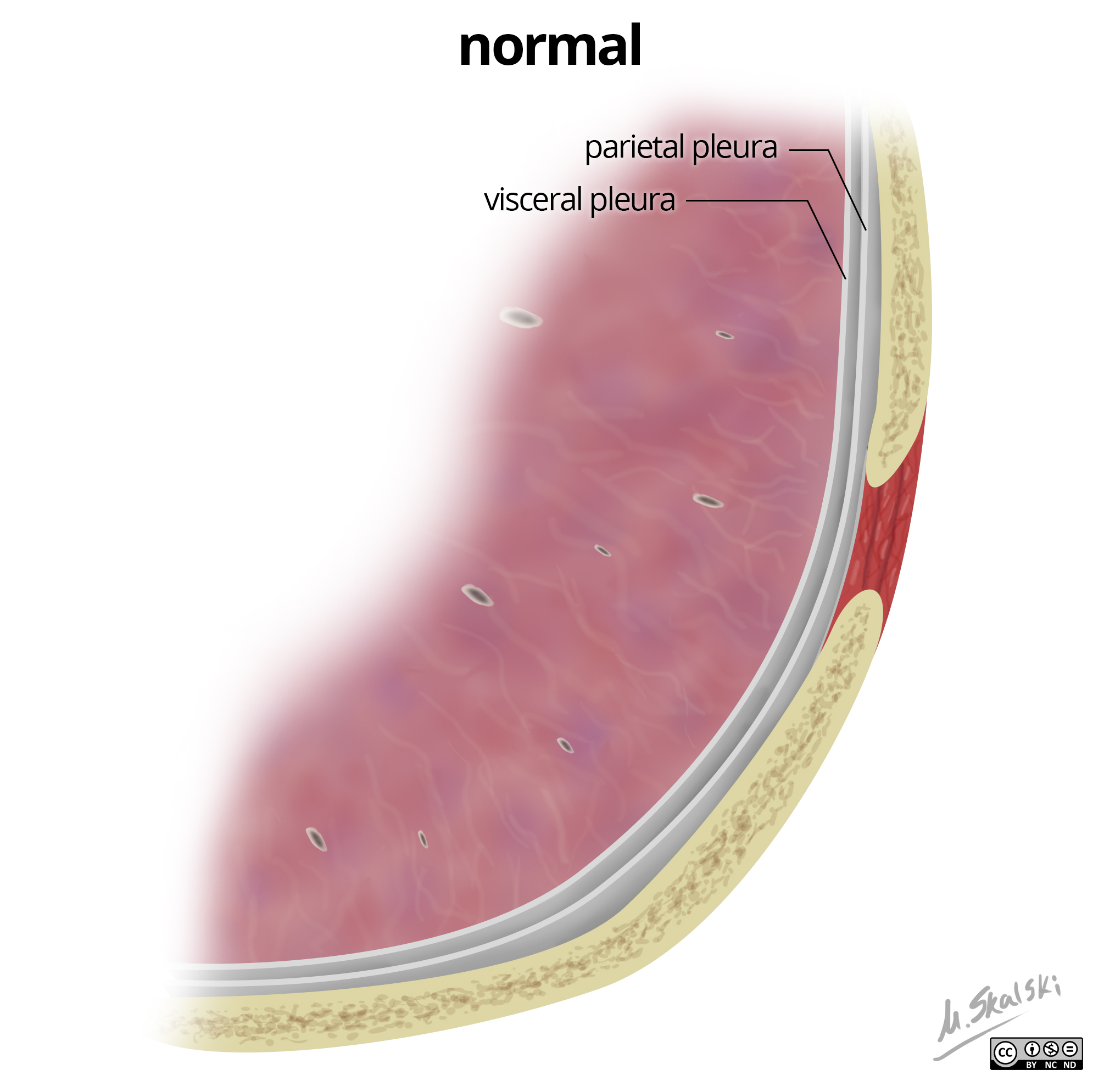
Structural Composition: Barrier, Mobility, and Protection The parietal pleura consists of a mesothelial lining over connective tissue rich in elastic fibers and collagen, providing durability without compromising flexibility.
Its parietal surface adheres firmly to surrounding tissues—anchoring lungs to the chest wall—but remains mobile enough to accommodate expansion during deep inhalation. In contrast, the visceral pleura is a simpler, more fragile layer composed only of a single layer of squamous mesothelial cells, unadorned by blood vessels or nerves. This minimalist design allows it to conform exactly to the lung’s contours, maximizing surface contact and minimizing inertial resistance.
Their shared visceral-pleural space—the intrapleural cavity—functions as a hydrostatic cushion. The fluid seeping between them (only 5–20 mL in adults) creates surface tension that prevents lung collapse while permitting gentle movement. “This balance of adhesion and fluidity is a marvel of evolutionary engineering,” explains Dr.
Rajiv Mehta, thoracic surgeon and pleural disease expert. “Disruption—whether from bleeding, infection, or mechanical trauma—can rapidly collapse a lung, demanding immediate intervention.”
The parietal pleura: a sensory sentinel.
While the visceral pleura operates with passive elegance, the parietal pleura is a bustling hub of afferent signaling. Its parietal nerve endings respond to changes in pressure, stretch, and chemical irritants—reacting swiftly to pathogens, inflammatory cytokines, or mechanical stress.
Clinically, this sensitivity translates into clear diagnostic markers: a sudden sharp pain upon deep breath often signals parietal irritation, guiding imaging and diagnostic choices. In pneumothorax, rupture of visceral pleural adhesion allows air to flood the space, stretching the parietal pleura and causing excruciating pain paired with impaired lung expansion.
Clinical Relevance: When the Pleural Barrier Fails Disorders involving the pleura reveal their essential roles. Pleural effusion—accumulation of fluid—exerts pressure on the visceral layer, impairing lung expansion and creating a visible bulge on imaging.
Meanwhile, empyema (infected fluid) may compromise visceral pleural integrity, requiringesthetic intervention. In malignant cases such as metastatic pleural involvement, tumor cells breach both layers, disrupting their cooperative dynamics and triggering painful effusions or fibrosis. “Putting these layers under the microscope changes the narrative,” says Dr.
Mehta. “We’re no longer just treating symptoms—we’re restoring a delicate physiological equilibrium.”
The interaction between parietal and visceral pleura extends beyond static anatomy; it plays a vital role in lung mechanics and disease progression. During inspiration, the pleural pressure gradient pulls the lungs outward, a process reliant on their synchronized responsiveness.
In conditions like pulmonary fibrosis or emphysema, stiffening of lung tissue alters how pleural forces translate into alveolar expansion, contributing to dyspnea and respiratory fatigue.
Even minor pleural abnormalities can cascade into systemic complications. Chronic pleuritic friction, often from autoimmune disease or post-surgical scarring, erodes the gliding capability of the layers, fostering adhesions that restrict motion and increase injury risk.
In.THORAX trauma, rupture of either pleural layer can unleash painful air or fluid into the cavity, demanding urgent surgical repair to reestablish homeostasis.
Understanding the parietal and visceral pleura’s distinct contributions empowers clinicians to diagnose with precision, treat with skill, and innovate with purpose. From guiding nerve-targeted pain relief to pioneering minimally invasive pleuro

Related Post

Kofi Siriboe Ethnicity: Unveiling The Cultural Roots Behind A Rising Hollywood Luminary

Decoding “Popular”: The Weeknd Unpacks Fame, Fear, and Identity in One Obsessive Track

Leta Ramirez: The Rising Star Redefining Entertainment

