Unlocking the Future: How AI-Driven Precision Diagnostics Are Revolutionizing Modern Medicine
Unlocking the Future: How AI-Driven Precision Diagnostics Are Revolutionizing Modern Medicine
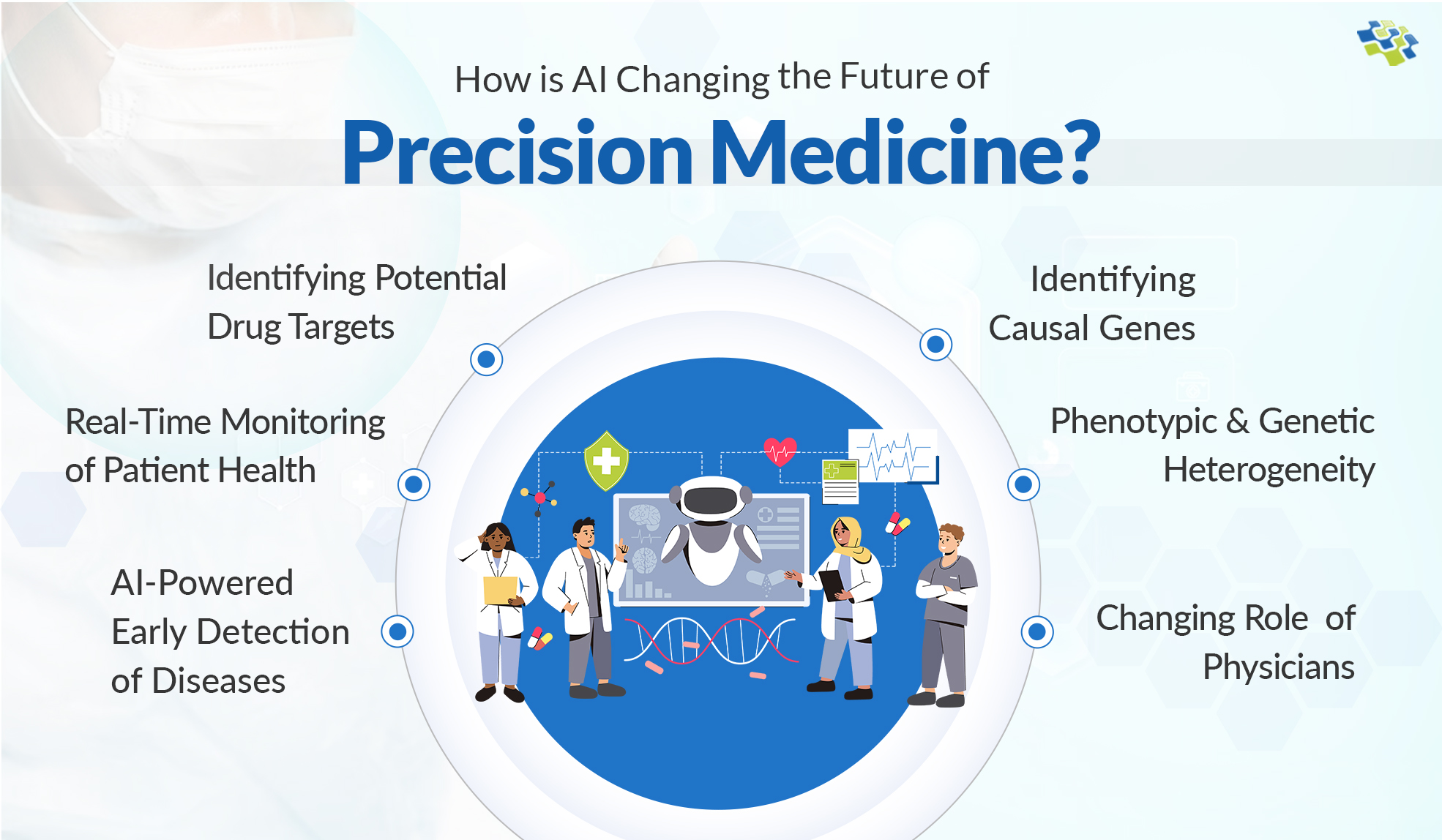
In a medical landscape undergoing unprecedented transformation, AI-powered diagnostic tools are emerging as critical forces reshaping how diseases are detected, analyzed, and treated. These systems leverage vast datasets, machine learning algorithms, and real-time analytics to deliver insights far beyond conventional methods—precisely where speed, accuracy, and personalization determine patient outcomes. From detecting subtle cancer markers in blood tests to predicting neurological decline before symptoms appear, the integration of AI into clinical workflows marks a paradigm shift in healthcare delivery.
The Science Behind Smart Diagnostics
Artificial intelligence in medicine hinges on deep learning models trained across millions of medical records, imaging studies, and genetic sequences.These algorithms identify complex patterns invisible to the human eye, enabling earlier and more accurate diagnoses. For instance, a 2023 study published in Nature Medicine demonstrated an AI model detecting early-stage lung cancer in CT scans with 94% accuracy—surpassing current clinical thresholds. This capability not only accelerates diagnosis but reduces misclassification errors that can delay critical treatment.
Key components fueling this revolution include: - **Machine learning classifiers** that parse imaging data, lab results, and patient histories - **Natural language processing (NLP)** extracting meaningful insights from clinical notes and pathology reports - **Predictive analytics** forecasting disease progression using longitudinal patient data - **Computer vision** enhancing radiology and dermatology imaging interpretation “AI doesn’t replace clinicians—it amplifies their judgment,” observes Dr. Elena Rajkomar, medical AI researcher at Stanford University. “By offloading repetitive analysis, doctors focus on empathy and decision-making, improving both efficiency and care quality.”
Transforming Disease Detection Across Specialties
AI’s impact manifests across medical disciplines, each sector experiencing distinct gains.In oncology, algorithms analyze histopathology slides to pinpoint tumor subtypes and mutation profiles, guiding targeted therapies with unprecedented precision. In cardiology, AI models evaluate electrocardiograms to predict arrhythmias or heart failure long before physical symptoms emerge. Dermatology benefits from real-time skin lesion analysis, where AI-powered apps assist in early melanoma identification, a shift that could save thousands of lives annually.
Mental health care is also advancing: digital biomarkers from voice analysis and wearable sensors help detect depression progression through AI-driven behavioral pattern recognition. According to a 2024 WHO report, such tools improve access to early intervention, particularly in underserved communities. Field | AI Application | Impact | |-------|----------------|------| | Oncology | Tumor classification, mutation prediction | Personalized treatment, reduced trial-and-error therapies | | Cardiology | ECG anomaly detection, risk stratification | Earlier arrhythmia alerts, reduced hospital readmissions | | Dermatology | Lesion classification, melanoma risk scoring | Improved early diagnosis accuracy | | Psychiatry | Behavioral tracking via voice and movement | Continuous mental health monitoring, reduced stigma | These innovations do not work in isolation.
They integrate with electronic health records (EHRs), creating feedback loops that refine predictions and treatment plans over time. As Dr. Rajkomar notes, “AI systems evolve with each patient interaction, becoming smarter and more tailored to individual biology.”
Addressing Barriers to Widespread Adoption
Despite remarkable progress, significant challenges slow AI’s full integration into healthcare.Data quality and bias remain critical concerns. Models trained on non-diverse datasets risk perpetuating disparities, particularly among minority and low-income populations. Transparency also ranks high—clinicians demand clear explanations for AI-generated recommendations to build trust and ensure accountability.
The regulatory landscape struggles to keep pace. While agencies like the FDA approve select AI-based diagnostic tools, standardization for validation, interoperability, and ongoing performance monitoring remains fragmented. Additionally, privacy concerns around patient data usage fuel cautious adoption, especially in regions governed by strict regulations such as GDPR in Europe or HIPAA in the U.S.
To overcome these hurdles, stakeholders emphasize collaborative frameworks. Hospitals must partner with tech developers, ethicists, and policymakers to co-design systems that prioritize equity, explainability, and security. Investments in diverse, high-quality datasets and open-source AI platforms can foster innovation while safeguarding patient rights.
Pioneering programs, such as Mayo Clinic’s AI ethics board and the EU’s trustworthy AI certification process, model this balanced approach. By embedding patient consent, audit trails, and bias mitigation protocols, these initiatives pave the way for scalable, responsible deployment.
The Future: Predictive, Personalized, and Preventive Care
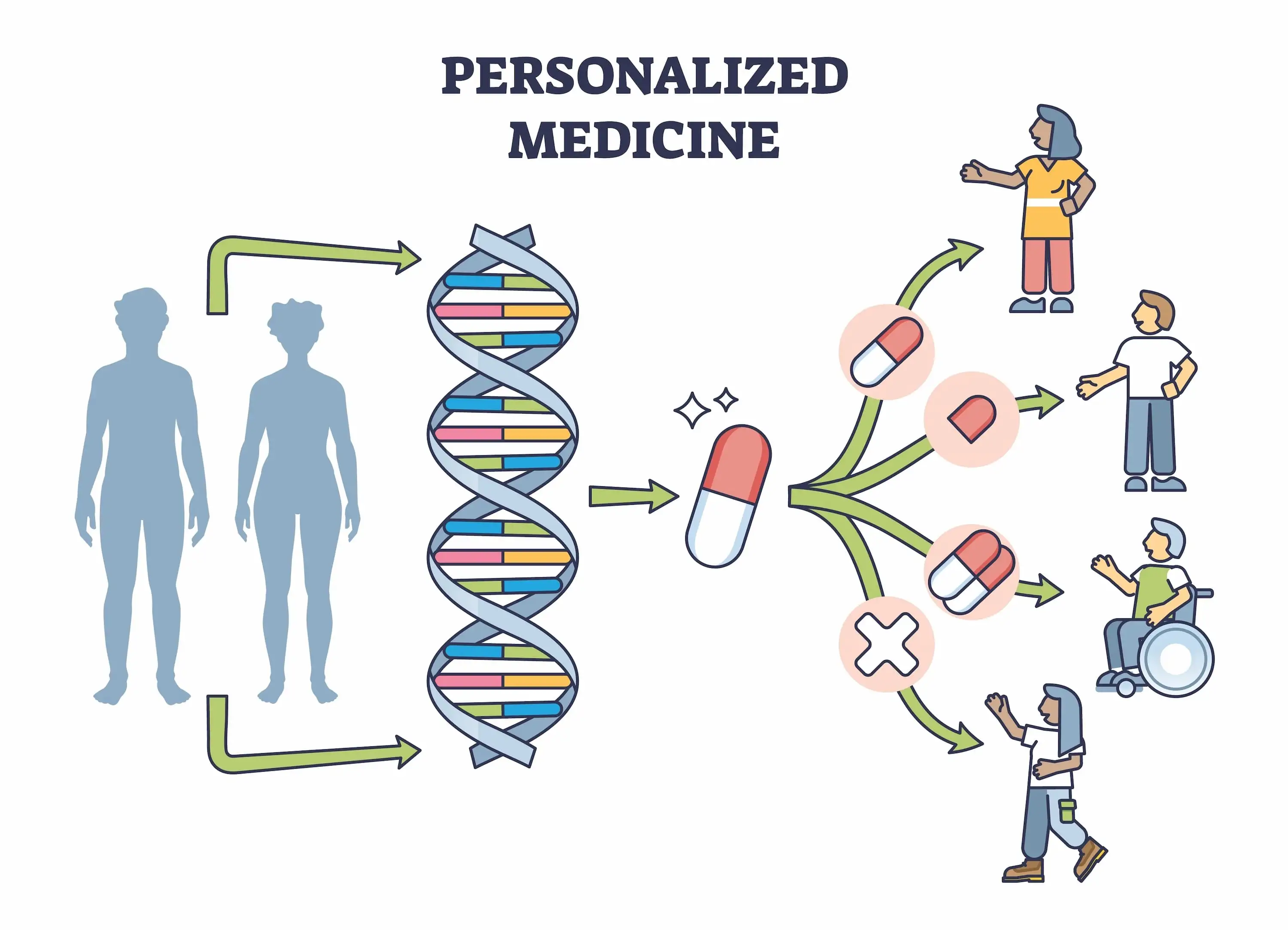
Looking ahead, AI-driven diagnostics will transcend current benchmarks, evolving toward proactive healthcare.Predictive algorithms will monitor vast data streams—genetics, lifestyle, environmental exposures—to flag risk long before disease onset. This shift from reactive to predictive medicine promises to reduce the burden of chronic illness, lower healthcare costs, and extend healthy lifespans. Imagine a future where smartphones track subtle biomarkers via non-invasive sensors, feeding real-time health insights into AI systems that recommend personalized prevention strategies daily.
Remote monitoring in rural or low-resource settings could bridge access gaps, democratizing elite diagnostic capabilities worldwide. “Medicine is becoming biology’s quantitative science,” asserts Dr. Carlos Santana, director of AI in precision medicine at MIT Medical.
“AI doesn’t just diagnose—it predicts, personalizes, and protects.” As technological capability accelerates alongside ethical stewardship, AI’s role in diagnostics is no longer supplemental—it is foundational. By merging human expertise with artificial intelligence, healthcare is poised to enter an era defined by precision, speed, and deeply personalized care, transforming patient journeys across the globe. In closing, the convergence of AI and medicine represents more than a technical advancement—it signals a fundamental reimagining of health itself, where early detection, targeted intervention, and continuous monitoring become the norm rather than the exception.
As innovations mature, their integration into clinical practice will not only save lives but redefine what it means to heal in the 21st century.

Related Post

Watch Hostages: The Pulse-Pounding Israeli Series Unraveling Terror, Resilience, and Human Drama

Marauders Meaning: Unpacking the Power Behind a Culture of Defiance and Identity
What Does B Stand For in Math? Decoding the Symbol That Defines Balance and Beyond

Unlock the Raw Soul of Protest: The Communist Slow Jams Director’s Cut Download Reveals Decades of Uncensored Resistance

