Pregnancy: Why Do Rising Red Blood Cells Define This Transformative Stage?
Pregnancy: Why Do Rising Red Blood Cells Define This Transformative Stage?
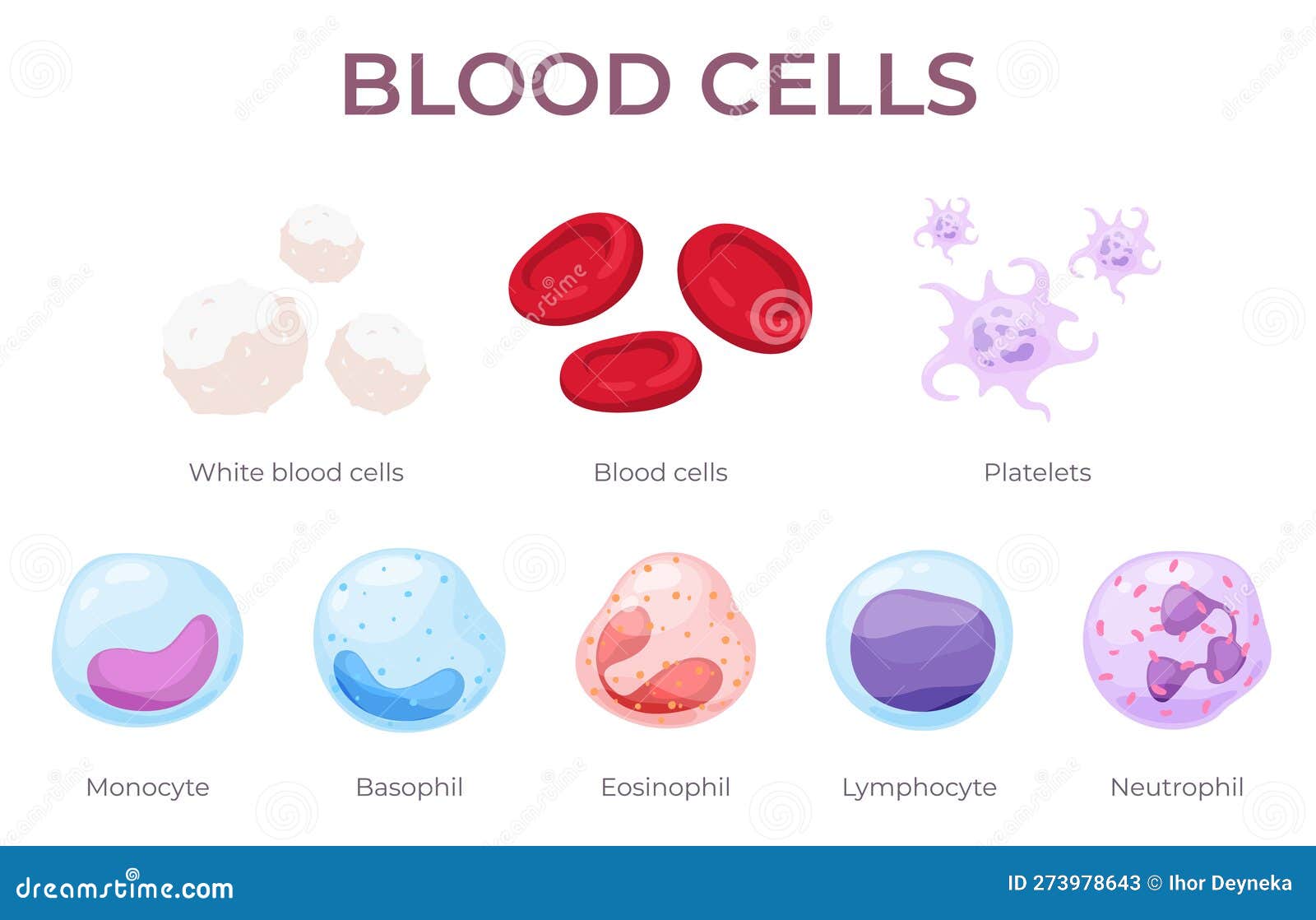
Pregnancy triggers a profound physiological transformation in a woman’s body, among which the dramatic increase in red blood cell (RBC) production stands out as both essential and well-orchestrated. Hemoglobin and RBC levels typically rise by 20 to 30% during gestation, a shift driven by complex hormonal signals and metabolic demands. Far from a passive process, this erythropoietic adjustment ensures adequate oxygen delivery to both mother and developing fetus, highlighting one of the body’s remarkable adaptive responses.
Understanding the causes behind this rise reveals a sophisticated interplay of hormones, nutrient availability, and blood volume expansion — a biological ballet essential for sustaining life through pregnancy’s key stages.
Hormonal Shifts: The Catalysts Behind Red Blood Cell Expansion
Central to the increase in red blood cells during pregnancy is the hormone erythropoietin (EPO), produced primarily by the kidneys in response to oxygen sensing.“EPO acts as the body’s natural signal to boost red blood cell production, rising steadily as the placenta takes over gas exchange duties,” explains hematologist Dr.
Elena Moralez. “This stimulation begins early in gestation, peaking in the second and third trimesters.” EPO levels rise by up to 50% in healthy pregnancies, prompting bone marrow to accelerate RBC synthesis. - EPO stimulates precursor cells in the bone marrow, enhancing their differentiation into mature red blood cells.
- This process not only increases total RBC count but also boosts hemoglobin concentration, normalizing oxygen-carrying capacity despite plasma volume expansion. - Without this hormonal drive, maternal tissues — especially the growing fetus — would face oxygen deprivation, risking developmental setbacks.
Blood Volume Expansion: A Dual Demand on the Circulatory System
Pregnancy induces a surge in overall blood volume, increasing by approximately 40–50% from baseline — a rise far outpacing the growth of red blood cells.This dramatic fluid expansion, rising at a rate of 500–1000 mL more blood by term, creates a relative dilution effect in plasma. While hemoglobin and hematocrit values may slightly drop, the absolute increase in red cell mass compensates for this dilution, ensuring sufficient oxygen transport. - The body prioritizes perfusion to the uterus, placenta, and fetal circulation, making this circulatory adaptation non-negotiable.
- Only a 20–30% rise in red blood cells maintains effective oxygen delivery despite plasma volume gains — a carefully balanced equilibrium. - This finely tuned expansion prevents maternal and fetal hypoxia, a critical safeguard throughout pregnancy.
Nutritional Requirements: Iron, Folate, and Vitamin B12 as Key Drivers
The escalating demand for red blood cells in pregnancy is grounded in the body’s heightened need for specific nutrients.Iron stands as the most pivotal: daily requirements jump from 18 mg to 27 mg to support expanded RBC synthesis. This element fuels hemoglobin formation, the oxygen-carrying protein within red blood cells.
Recent findings confirm that iron deficiency during pregnancy — affecting up to 30% of women globally — directly correlates with reduced RBC expansion and elevated risk of anemia and preterm delivery.
- Folate and vitamin B12, essential for DNA synthesis in rapidly dividing red blood cell precursors, are equally critical. - Deficiencies in these vitamins impair erythropoiesis, limiting RBC growth and potentially straining placental function.
Dietary sources like lean red meat, leafy greens, legumes, and fortified cereals are strongly recommended, though supplementation is often necessary under medical supervision.
دراسات أظهرت أن المكملات الغذائية الموجهة للحديد، الفولات، وفيتامين ب₁₂ significantly improve maternal RBC counts, reinforcing the link between nutrition and effective erythropoiesis during pregnancy.
Age, Parity, and Individual Variability in Red Blood Cell Dynamics
The magnitude of red blood cell increase during pregnancy varies subtly across women, influenced by age and prior reproductive history.Younger, nulliparous women — those with no prior pregnancies — often exhibit greater RBC gains, possibly due to a less complex vascular history and primed bone marrow response.
In contrast, multiparous women may experience a slightly tempered erythrocyte expansion, reflecting prior hormonal and circulatory adaptations. - Age-related declines in bone marrow plasticity and iron stores modestly reduce peak RBC elevations in older mothers, though this remains context-dependent. - Chronic conditions like inflammation or renal insufficiency can further perturb erythropoietin signaling, altering expected RBC trajectories and requiring close monitoring.
Recognizing this individual variability ensures personalized care, avoiding unnecessary interventions while safeguarding both mother and child.
The Physiological Priority: Ensuring Oxygen Supply to Fetus and Maternal Tissues
The primary biological imperative behind rising red blood cells in pregnancy is ensuring adequate oxygen delivery — a non-negotiable support for fetal development and maternal health.The placenta acts as a high-demand interface, extracting oxygen from maternal blood to sustain the fetus’s rapidly growing tissues.
Even minor disruptions in RBC expansion risk compromising this critical exchange.
Clinical studies underscore that women with insufficient RBC responses face higher risks of intrauterine growth restriction, preterm birth, and postpartum complications. - Conversely, beneficent elevation in RBC mass improves placental efficiency, fetal hemoglobin saturation, and long-term neurodevelopmental outcomes.
This oxygen delivery mechanism exemplifies nature’s precision: a dynamic, responsive process fine-tuned by evolution to protect two lives.
While the rise in red blood cells may seem like a routine byproduct of pregnancy, it represents a profound, hormone-guided adaptation essential for sustaining life through this transformative period. From EPO-driven marching of bone marrow to the nutritional foundations and blood volume dance, every aspect converges on one purpose — ensuring that both mother and child receive the oxygen they need to thrive.
This intricate balance, honed by biology and refined through millions of years of human evolution, underscores why red blood cell expansion remains not just a statistic, but a cornerstone of maternal-fetal wellness.



Related Post

Decode Eigenvectors: The Essential Step-by-Step Guide to Finding Them in Linear Algebra

Rashmika Movies: The Unstoppable Force Reshaping Bollywood’s Landscape

Jeanette Dousdebes Rubio: Architect of Equitable Health Policy in Costa Rica
Hockey Team Logos A Visual Guide With Names: The Symbols That Define a Franchise

